.png)
.png)
.svg)
.svg)
Neuroengineering the brain
Neuroengineering the brain
Reframing the brain as a data organ
Since the brain is a data organ, it needs a digital brain interface
The brain is fundamentally an information processing system. It receives information about the world through the senses, processes that information, and sends control signals to the muscles to respond to the environment. In the same sense that the heart is a “fluid dynamics organ,” and the kidneys are a “filtration organ,” the brain is a “data organ.” When a heart fails, it may be assisted by a pump. When the kidneys stop functioning, a dialysis machine may help with filtration. We need an analogous solution for brain conditions that do not have immediate biological solutions: Interfacing with a data organ requires a data interface. This is the foundation of neuroengineering, to develop a human interface device that serves seamlessly as a brain interface.
The staggering scope of neurological and brain-related health conditions
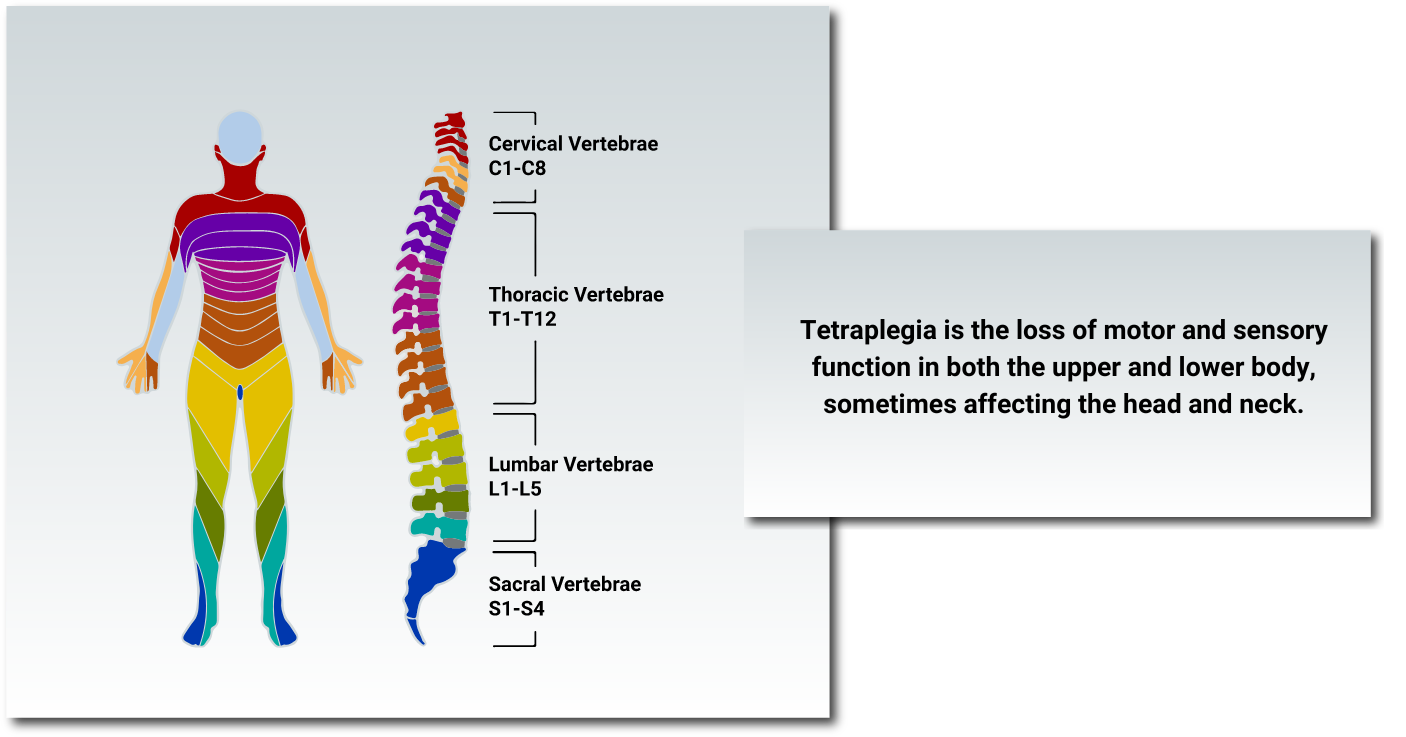
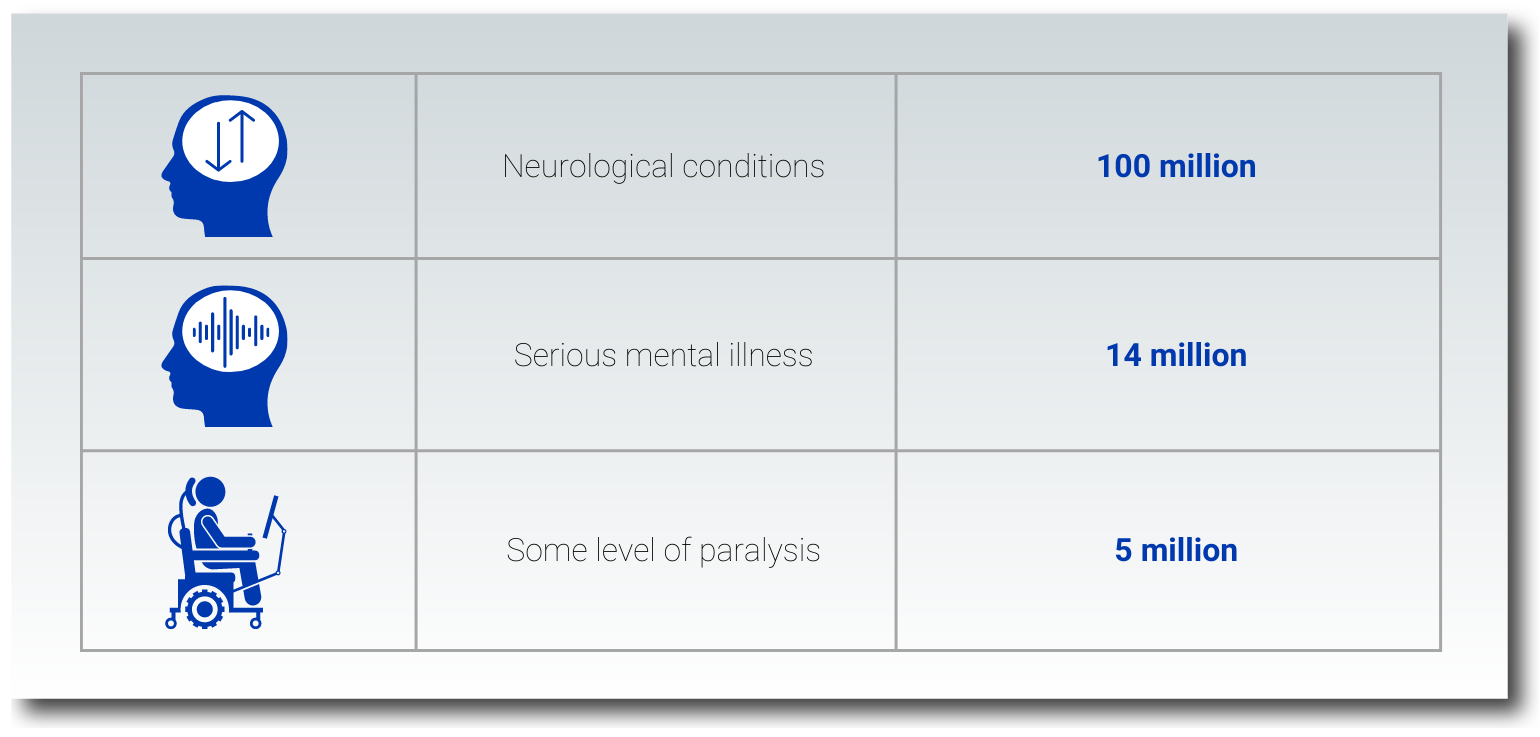
Globally, one billion people suffer from a neurological disorder, ranging from Parkinson’s disease or multiple sclerosis (MS) to epilepsy or dementia. In the United States alone, 100 million people–approaching one-third of the population–are affected by one of over 1000 neurological conditions. Paralysis, a neurological condition resulting most commonly from spinal cord injury (SCI) or stroke, poses a significant disease burden. Over 5 million Americans—or 1 in 50—live with some level of paralysis; of those with SCI, incomplete or complete tetraplegia affects 48% or 12%, respectively. Furthermore, disabling blindness and deafness, which often arise because of neurological disease or injury, each affect around 5% of Americans.
In addition to the neurological conditions above, there is a 45% lifetime incidence of mental illness among Americans, most commonly anxiety, depression, obsessive compulsive disorder (OCD), or post-traumatic stress disorder (PTSD). In 2020, about 14 million Americans were living with a serious mental illness.
The brain as a data organ: A case for neuroengineering
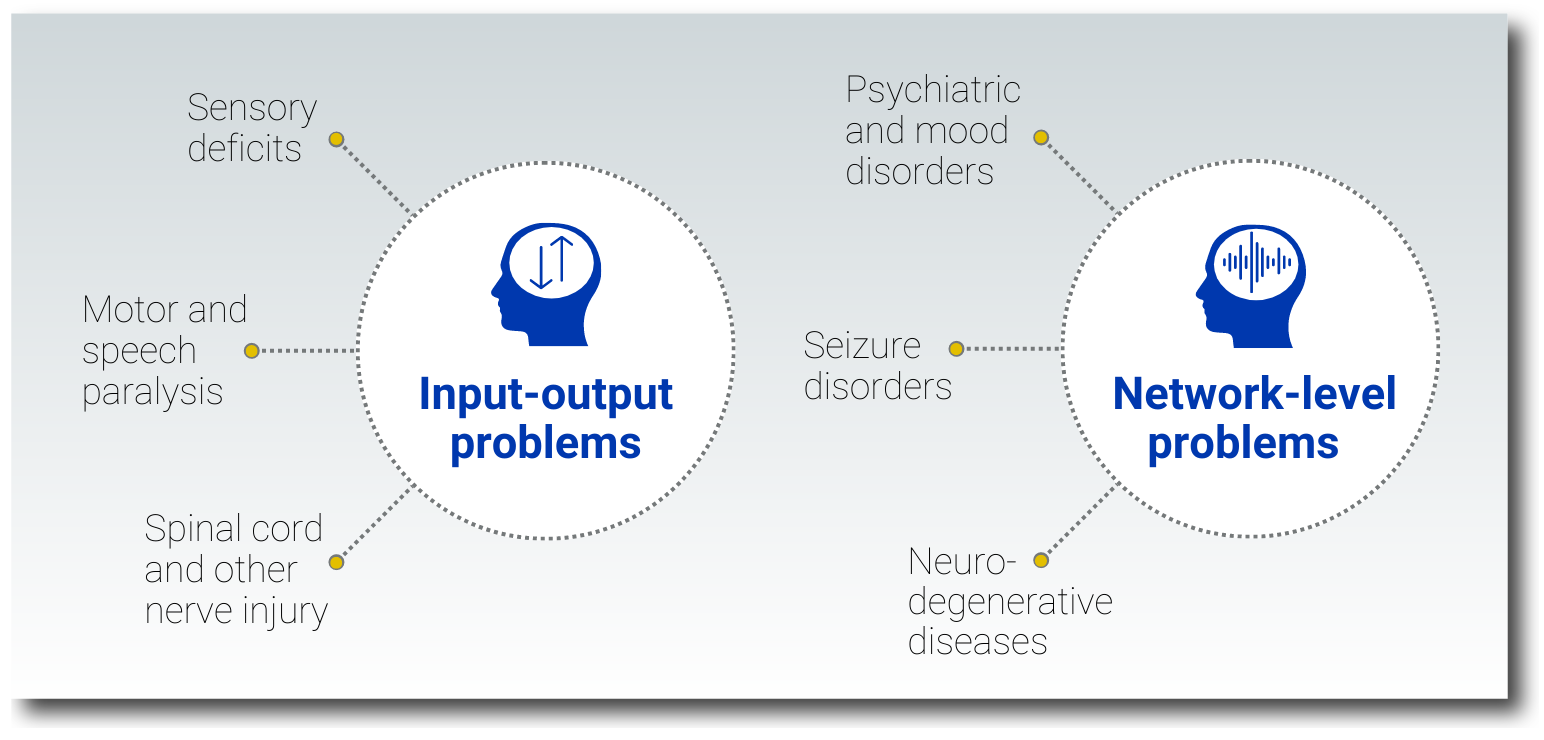
By thinking of the brain as an information processing system, we may reframe these widespread and varied conditions—and their treatments—in terms of accessing and handling data. In this analogy, just as a computer may encounter problems sending, receiving, or processing data, the brain’s input-output functionality may break down, or dysfunction may arise within the brain’s internal network. This reframing can provide new insights into neurological and brain-related conditions and open the door to neuroengineering solutions that apply human interface devices to the treatment of brain disorder.
Input-output problems and the need for brain interfaces
The brain engages in constant conversation with the rest of the body via the central and peripheral nervous system. Signals from sensory organs tell the brain about the world around us, and the brain processes these signals using cognition. In turn, the brain sends signals to the muscles to control movement, effecting change in the physical world. Understandably, when these communication channels are compromised through injury or disease, sensory or motor impairment follows, leading to conditions like blindness, deafness, or paralysis. One of the most life-altering consequences of severe paralysis is the inability to communicate through speech, writing, or hand signs, resulting in the loss of autonomy and social connection.
Network-level problems in the brain’s data system
Many neurodegenerative disorders including Alzheimer’s, MS, and Parkinson’s disease have been tied to dysfunctional connectivity within the brain network.
Similarly, some mood and psychiatric disorders are associated with network-level dysfunction, with different depression subtypes correlating to identifiable network patterns. Significantly, taking a network view of these brain conditions allows doctors and scientists to consider these network patterns as biomarkers for diagnosing disease and evaluating the efficacy of treatments.
Current therapies neglect brain data
How we treat input-output problems without brain interfaces
At present, modalities for treating conditions that arise from input-output problems are experimental or provide only rudimentary restoration of function. For instance, cochlear implants, which translate acoustic energy into electrical signals that are used to stimulate the auditory nerve, have seen improving performance over the past few decades. The more-recently developed Second-Sight retinal prosthesis replicates visual perception by simulating neurons in the eye, resulting in a crude (60 x 60 pixel) grayscale image. (Note that neither of these technologies directly stimulate the brain. Experimental treatments that directly address input-output problems are covered below.)
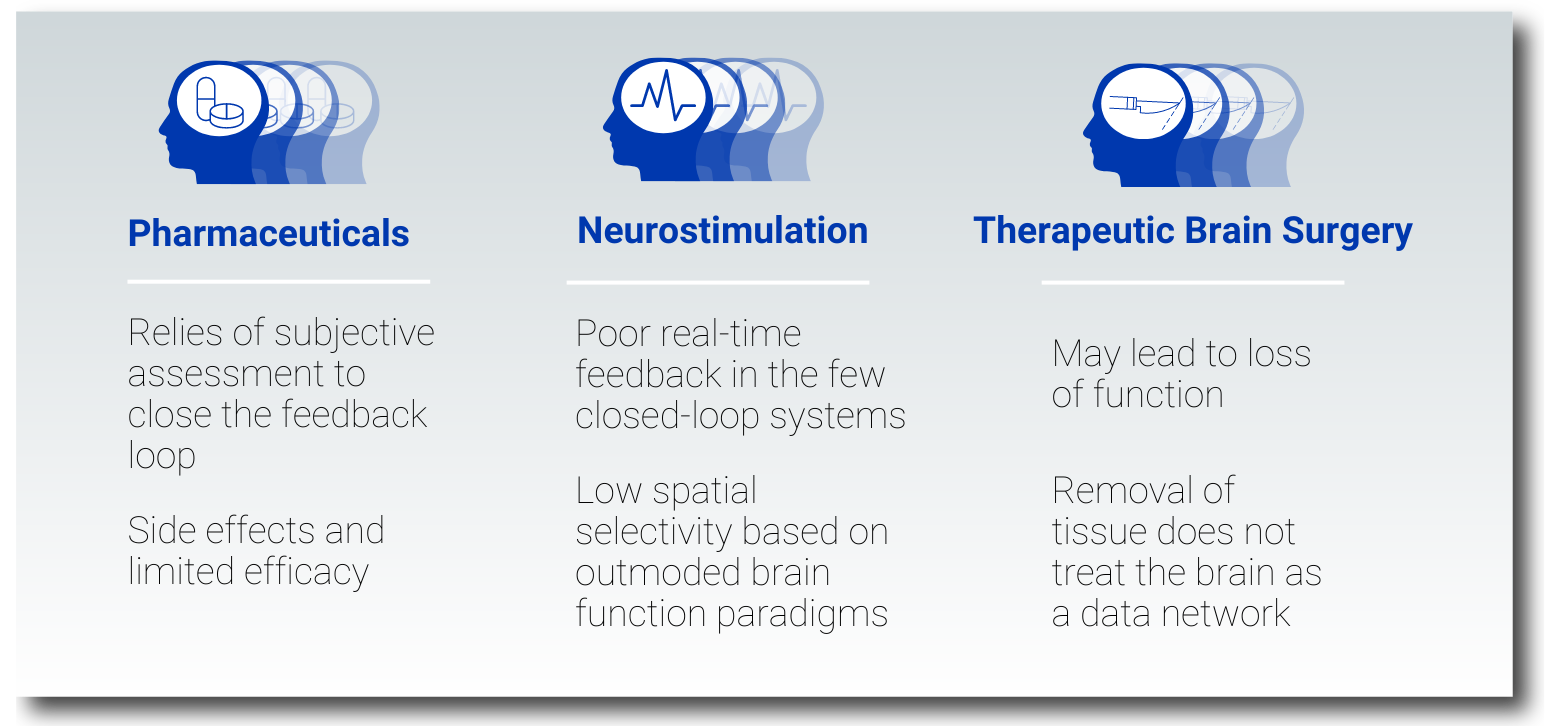
How we treat network-level problems with limited neuroengineering approaches
Most commonly, network-level problems in the brain are treated with pharmaceuticals, neurostimulation devices, and therapeutic brain surgery. In all instances, these therapies do not address the brain as a data system, leaving patients with significant unmet needs.
Pharmaceuticals and their limitations
The drawbacks of medications, including side effects and lack of efficacy, especially for psychiatric disorders, are well-known. This can be attributed to the fact that these small, often broad-acting molecules travel throughout the brain without prejudice, where they bind to receptors and potentially disrupt network function. Furthermore, even when pharmacological control of a condition is possible, evaluation of effectivity is difficult without feedback. Currently, these treatments rely on slow, subjective clinical assessment to close the feedback loop, rather than measurable biomarkers in the brain’s data network.
Neurostimulation without adequate brain data feedback
To modulate dysfunctional neural circuitry, neurostimulation therapies apply electromagnetic energy to specific parts of the brain. While this treatment has seen clinical success for some conditions, like deep brain stimulation (DBS) for Parkinson’s disease, it has low spatial selectivity and is based on outmoded, oversimplified notions of brain network function. These systems either have no or limited recording capabilities; again, poor real-time data feedback from the brain further limits the effectiveness of this approach.
Therapeutic brain surgery and its drawbacks
Finally, therapeutic brain surgery involves the coarse removal of tissue with little regard for the brain as an interconnected data network. Besides being of limited value for most brain-related disorders, in conditions where the treatment is effective, the procedure may lead to unintended loss of function.
BCI and neuroengineering research show the possibility of using brain data
Brain-connected devices, and specifically brain-computer interfaces (BCI), have demonstrated capabilities in the clinical research setting for treating speech and motor impairment and mental illness. These devices tap directly into brain data, allowing researchers to apply digital technologies to address complex medical problems. In this way, neuroengineering is transforming the BCI into a clinically useful human interface device; a scalable brain interface.
Solutions to input-output problems via brain interfaces
By establishing a lingua franca among neural and digital signals, a brain computer interface (BCI) creates a channel for passing brain data from the biological to the technological realm, and vice versa. In someone with paralysis, for instance, the interface might gather signals from neurons in the motor cortex and use this data to guide a wheelchair, exoskeleton, or prosthetic limb. Indeed, BCI control of robotic prosthetics has been achieved in clinical trials. Researchers are also honing BCI systems that address both the motor and sensory deficits that come with paralysis; these bidirectional systems provide both neurosensing and neurostimulation.
Similarly, researchers have demonstrated BCI solutions for patients whose motor impairment means they cannot effectively communicate through speech or typing. By translating the data from neural activity into intended actions and words, these systems allow patients to control a computer cursor for applications like typing. More recent studies have utilized the direct decoding of imagined handwriting and speech.
Neuroengineering solutions to network-level problems
As mentioned previously, numerous neurological and mental health conditions are associated with changes in the brain’s network, manifesting as cognitive, mood, or movement disorders. This suggests an alternate pathway for treating these conditions: addressing the problem at the level of neural activity in the brain. New experimental treatments are doing just that.
For instance, by combining neurostimulation with brain data gathered through BCI, researchers have successfully treated patients with depression and OCD—conditions that are debilitating without proper management.
“She tried nearly every treatment: roughly 20 different medications, months in a hospital day program, electroconvulsive therapy, transcranial magnetic stimulation. But as with nearly a third of the more than 250 million people with depression worldwide, her symptoms persisted. Then Sarah became the first participant in an unusual study of an experimental [DBS] therapy. Now, her depression is so manageable that she’s taking data analysis classes, has moved to her own place and helps care for her mother, who suffered a fall.”
- A ‘Pacemaker for the Brain’: No Treatment Helped Her Depression — Until This, New York Times
As discussed previously, certain brain network patterns are tied to specific depression sub-types. Likewise, researchers have also identified certain patterns that correlate to specific mood states and, in turn, have demonstrated a mood state “decoder”. Access to this type of brain data could close the feedback loop gap that currently hinders effective treatment.
“Our goal is to create a technology that helps clinicians obtain a more accurate map of what is happening in a depressed brain at a particular moment in time and a way to understand what the brain signal is telling us about mood. This will allow us to obtain a more objective assessment of mood over time to guide the course of treatment for a given patient.”
- Maryam Shanechi, research lead in the “mood decoder” study)
New neuroengineering solutions for accessing brain data
Despite the amazing BCI capabilities that have been demonstrated in these academic studies, the future holds even more promise. Currently, the highest-performing BCI systems for motor control or communication require one or more data ports to penetrate the patient’s scalp and are only approved for short-term investigational use. Similarly, BCI mental health treatments described above were based on first-generation neuromodulation devices and low resolution brain data.
At Paradromics, we are translating this academic experience into a marketable, therapeutic product: a data interface with the brain meant for advanced medical applications. This represents the future of neuroengineering, where a high-performance human interface device evolves into a scalable, safe, and effective brain interface.
%20(1).svg)

.svg)